Patient information
Patient information
Graft selection in anterior cruciate ligament reconstruction
Bone-Patella Tendon-Bone vs. Hamstring Grafts
R.L.Morgan-Jones, M.J.Cross
IS THE GRAFT CHOSEN FOR ACL RECONSTRUCTION IMPORTANT? YES!
The graft chosen should;
1) Provide adequate fixation to allow rehabilitation,
2) Allow anatomic re-creation of the ACL in both size and location
3) Have adequate initial strength to survive the uncertainties of graft regeneration.
Bone-Patella Tendon-Bone (B-PT-B) grafts have the best initial fixation by using interference screws to produce rigid bone-to-bone fixation. Hamstring fixation is soft tissue to bone via sutures and is less rigid.
Both B-PT-B and Hamstring grafts should allow re-creation of the ACL in both size and location although this is largely dependent on the experience and expertise of the surgeon.
Both B-PT-B and Hamstring grafts need to undergo regeneration or they will fail. The initial fixation and tensioning of the graft both effect the biology of healing. In this respect B-PT-B graft has an advantage and theoretically has the best chance of functional regeneration.
Bone-Patella Tendon-Bone Grafts
Advantages: Excellent initial and long-term fixation, better overall stability
Disadvantages: Increased anterior knee pain, 2 incisions (plus arthroscopy portals)
Hamstring Grafts
Advantages: Lower incidence of anterior knee pain and crepitus, Single incision (plus arthroscopy portals)
Disadvantages: Less secure initial and long-term fixation, increased knee laxity after reconstruction
In prospective studies comparing B-PT-B vs. Hamstring grafts it was found that both grafts are good choices in ACL reconstruction but that B-PT-B graft provides more overall knee stability than hamstring grafts (Otero et al., Arthroscopy). At present the “Gold Standard’ ACL reconstruction is B-PT-B Graft (Johnson R.J., The Knee)
Your anaesthetic
WHAT TYPES OF ANAESTHETIC ARE COMMONLY USED?
1. Regional anaesthesia
The most common regional anaesthetic that we use is a spinal anaesthetic. This involves injecting a small volume of anaesthetic near to the nerves in the lower back (see picture),
which will feel totally numb from the waist downwards. This feeling will last for between 2-4 hours. It is possible to remain awake during your operation (you will not be able to see any of the operation) however many people prefer to have some ‘sedation’. If this is your preference we are usually able to give you drugs that will help you feel sleepy and relaxed whilst your operation is taking place.
This is the usual anaesthetic I will use for your knee replacement (usually in combination with a nerve block)
The next most common regional anaesthetic is an epidural (it is similar to, but not identical with. a spinal). A small plastic tube (an epidural catheter) passed through a needle and placed close to where the nerves leave your spine. Local anaesthetic and other pain relieving drugs are injected through this tube and will numb the lower half of your body. It is generally used for operations which will take longer (say over 3 hours) or operations, which are expected to be very painful afterwards. The catheter will remain in your back (you will not feel it there) and we can use a machine to keep giving you pain killers through this tube for up to 72 hours after your operation.
2. General anaesthesia
This is a state of controlled drug-induced unconsciousness. Anaesthetic drugs injected into a vein are carried to the brain by the blood. They stop the brain recognising messages coming from the nerves into the body.
This is the usual anaesthetic I will use for your arthroscopy or ACL repair.
3. Nerve blocks
This is an injection of local anaesthetic close to the nerves, which go to your leg. Part of your leg will feel numb and pain free for up to 24 hours after your operation. This means that you should need less strong pain relieving medicine both during and after your operation which should make you feel less drowsy and/or sick afterwards.
If you are having a knee replacement or an ACL repair your will usually have a nerve block in addition to your regional or general anaesthetic to give you extra pain relief.
4. Local anaesthesia
A local anaesthetic numbs a small part of your body. It is used when the nerves can be easily reached by drops, sprays, injections or ointments. You stay conscious but free from pain. If you are having a knee arthroscopy we usually inject local anaesthetic into the joint to provide extra pain relief.
The choice of anaesthetic depends on many things including;
• The type of operation you are having
• Your general health
• Your physical condition
• Your preferences and the reasons for them
• My recommendations and the reasons for them
Side effects, complications and risks
Using modern anaesthetic techniques, serious problems are uncommon. Risk can never be removed completely but modern equipment, training and drugs have made anaesthesia a much safer procedure in recent years.
The risk to you as an individual will depend on;
• Whether you have any other illnesses
• Personal factors, such as whether you smoke or are overweight
• Surgery which is complicated, long or done in an emergency
Everyone varies in the risk they are willing to take. I will be happy to advise you if you are concerned.
Arthroscopic knee procedures
KNEE SYNDROMES & ARTHROSCOPIC KNEE PROCEDURES
R.L.Morgan-Jones, M.J.Cross O.A.
There are many knee operations that can be performed using an arthroscope. Most operations can be done as a day-case procedure although many patients require a period of muscle strengthening afterwards to obtain the best outcome. Below is an outline of the commonest “knee syndromes” and the arthroscopic procedures used to treat them.
Medial meniscal syndrome 1, 2 & 3
1. Locked knee
A torn meniscus can displace into the knee joint causing a mechanical block to extension and resulting in pain and muscle spasm. The classic type of meniscal tear producing a locked knee is the “Bucket Handle” tear. The torn meniscus remains attached front and back allowing the central torn portion to flip into the knee joint like the handle of a bucket. As the pain and spasm reduce the displaced meniscus can drop back allowing the knee to move freely again. This mechanical “locking” of the knee can be an intermittent feature with symptomless periods of in-between episodes.
2. Medial pain syndrome
The gradual onset of pain aggravated by twisting, squatting and catching your toe; as well as pain at night when you sleep on the side with legs together. This is typical of a cleavage tear of the medial (inner) meniscus which can intermittently be “pinched” by the knee joint as it flexes or twists suddenly. In-between episodes the torn portion of meniscus can fold away under the untorn meniscus and the knee become pain free.
3. Lateral pain syndrome
The triad of pain in the lateral (outer) joint line, radiation up into the thigh and down into the lower leg, and exacerbation on ascending stairs are all associated with a torn lateral meniscus. The clinical sign of a meniscal ‘pseudocyst’ is a lump in the lateral joint line, tender to touch and varying in prominence according to the degree of flexion of the knee. The ‘pseudocyst’ results from the torn meniscus folding in on itself.
Meniscectomy
There are two menisci in every knee, the medial (inside) and the lateral (outside). Menisci can be damaged acutely when the knee sustains a sudden forced flexion and twisting strain, or chronically as part of degenerate changes within the knee (‘wear & tear’). The meniscus has little blood supply, except along the periphery where it attaches to the joint capsule, and therefore is unlikely to heal. A torn meniscus causes mechanical interference in the knee joint. This may result in the knee ‘locking’, preventing full extension. Recurrent displacement of a torn meniscus can produce damage to the smooth articular surface of the knee resulting in long-term degeneration.
Torn menisci can be removed by arthroscopy leaving the undamaged, stable portion behind. Occasionally a meniscus is torn along its peripheral attachment where there is a reasonable blood supply. This type of tear can sometimes be repaired allowing the meniscus to heal.
Anterior knee pain
Many people, of all ages and sporting activity, have pain generally located to the front (anterior) of the knee. This is caused by a relative weakness of the Quadriceps muscles in front of the thigh and tightness of the Hamstring muscles behind the thigh. In biomechanical terms this has the effect of walking on a permanently bent (flexed) knee. This increases the pressure on the patella and produces anterior knee pain. Occasionally this is precipitated by a minor injury, which results in residual Quadriceps weakness after the original injury has healed. Often however there is no prior accident or injury.
The solution to this problem is Quadriceps strengthening and Hamstring stretching. Quadriceps strengthening is best achieved by repetitive straight leg raising. Quadriceps exercises, which involve knee flexion, should be avoided, as flexion exercises will aggravate the pain. Hamstring stretching is equally important to reduce the flexion force around the knee. These exercises take at least 6 to 12 weeks to work and thereafter should be part of a patient’s daily routine.
Lunge lesions
The “lunge lesion” is an isolated injury to the femoral articular cartilage in the groove (Trochlea) through which the patella runs during knee flexion. It is the result of high shear and compressive forces produced by deceleration of the flexed knee, with co-contraction of the hamstrings and quadriceps muscle groups. Classically during a lunging motion as often occurs in sports such as squash, tennis, and netball. This roughened articulating area produces a painful, grinding sensation as the flexes leading to joint irritation and swelling. In severe cases this damaged area requires an arthroscopic chondroplasty to smooth the roughened articular cartilage. All patients however will require an exercise programme of Quadriceps strengthening and Hamstring stretching to protect against further injury.
Chondroplasty
The weight-bearing surface of the knee joint is covered in a highly specialised articular hyaline cartilage. This surface allows near friction free movement and absorbs the normal loading that occurs with daily activities. If an acute injury or chronic degeneration damages this surface, the cartilage roughens and causes local irritation. Sometimes a crackling sound or sensation may be present. As the cartilage deteriorates the knee itself can become swollen as the synovial joint lining produces increased amounts of synovial fluid to try and lubricate the knee.
These rough areas of articular cartilage can be smoothed by using an arthroscopic ‘shaver’. This removes any loose or roughened areas leaving a smooth articulating surface, thus reducing the local irritation.
Microfracture
When the articular hyaline cartilage is damaged to the extent that the underlying bone is exposed chondroplasty by itself is insufficient. In these cases we need to promote new cartilage formation in the damaged area. This is done by breaking through the exposed bone, using a bone awl, to the underlying blood supply (microfrature). The bleeding bone surface will ‘heal’ by the formation of a new cartilage layer. This new cartilage is called fibrocartilage and forms a new smooth surface, although it lacks some of the special properties of the original hyaline cartilage.
Notchplasty
In knees, which already have osteoarthritis, the joint forms new bone called osteophytes. These can often be felt on the edge of the knee joint as a bony lump. If osteophytes form in the middle of the knee joint they can prevent full knee extension, which in turn prevents muscle strengthening around the knee. In some patients it is possible to remove these central osteophytes arthroscopically and improve knee extension.
Removal of loose bodies
A piece of bone or cartilage can be broken off during an injury or as part of a more general degeneration and form a ‘loose body’ within the knee. Loose bodies can remain symptomless for long periods but can cause sudden attacks of pain and locking. Usually the locking is only momentary and the knee can be ‘wriggled’ free.
Loose bodies can be removed at arthroscopy although they can often be difficult to find.
Potential complications of total knee replacement
Rhidian Morgan-Jones
SPECIFIC COMPLICATIONS
Infection
Despite surgery under sterile conditions, infection is still a potential complication of all operations. Post-operative infection maybe:
a) Superficial wounds only and usually settles with antibiotics.
b) Deep involving the joint. Requires further surgery to debride the joint and intravenous antibiotics. Often a revision operation, with exchange of implants, is needed to eradicate the infection
Deep venous thrombosis & pulmonary embolus
A blood clot in the deep veins of the calf or thigh is a complication of any lower limb surgery. A blood clot that breaks-off and travels to the lungs is called a Pulmonary Embolus. This is a rare but life threatening complication. The treatment is anti-coagulation for 3-6 months.
Stiffness
It requires hard work after knee replacement surgery to achieve the maximum possible range of movement. Occasionally the knee can become stiff due to excess scar formation (Arthrofibrosis). This may require later surgery to excise the deep scar tissue.
Losening
The new knee joint is initially a press-fit or cement grout onto the bones. Over a period of years the bone-implant interface may breakdown leading to loosening of the knee replacement. Often this is associated with increased wear of the polyethylene insert, which sits between the metal implants to allow movement. A loose knee replacement may need revision surgery to replace the components.
GENERAL COMPLICATIONS
Wound healing
All knee replacements are performed through open incisions in front of the knee. The first priority after surgery is to ensure the wounds heal adequately. Delayed wound healing is sometimes seen in patients with systemic diseases such as Rheumatoid Arthritis or inpatients that have been taking Steroids for any reason.
Haemarthrosis
Bleeding within the knee joint can complicate any surgical procedure. A haemarthrosis will usually respond to ice, rest and physiotherapy but can lead to delayed recovery and joint stiffness.
Nerve Injury
Small areas of numbness may be associated with the operative incisions. The numbness is usually temporary. Occasionally wounds can become painfully sensitive, although this normally settles with time.
Reflex sympathetic dystrophy
Reflex Sympathetic dystrophy is a little understood condition, which can complicate any operation. It consists of regional pain, swelling, sweating and stiffness due to local overactivity of the sympathetic nerves triggered by surgery, however minor.
Complications of ACL Reconstruction
POTENTIAL COMPLICATIONS OF ARTHROSCOPIC ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION
Rhidian Morgan-Jones
SPECIFIC COMPLICATIONS
Patellar fracture
Use of the bone-patellar tendon-bone graft may result in patellar fracture. This can occur at the time of harvest or later during rehabilitation. Patellar fracture may require operative reduction and internal fixation. It may result in chronic patello-femoral pain. This rare complication has been reported in the medical literature but has never occurred in my practice to date.
Patellar tendon rupture
This rare complication has been reported in the medical literature but has never occurred in my practice to date.
Patellar tendonitis & calcification
Patellar tendinitis may occur during the rehabilitation period. Symptoms usually resolve with rest, anti-inflammatories and physiotherapy. Local calcification may occur within the patellar tendon at the site of graft harvest and may produce local irritation. This rare complication has been reported in the medical literature but has never occurred in my practice to date.
After harvest, local pain and bruising is normal along the line of the hamstring (rear of the thigh). During the weeks that follow surgery, the remaining hamstring tendons may rupture, leading to pain and immobility.
Graft fixation screws
Local irritation from the screws used to secure and tension the graft may necessitate screw removal. This complication is irrespective of graft choice.
Graft failure
Cruciate ligament reconstructions have excellent initial fixation and stability. In the long term however the graft relies on revascularisation to allow permanent bone growth and new-ligament formation. This takes approximately 6 months but can continue for up to 2 years after surgery. Failure of revascularisation can lead the graft to weaken, possibly leading to recurrent symptoms of instability. This complication is more common amongst hamstring grafts and leads to a higher failure rate than seen with bone-patellar tendon-bone grafts.
Stiffness
Stiffness (loss of motion) may result from many causes including prolonged immobilisation, reflex sympathetic dystrophy, infection and pain. Technical problems related to graft placement might lead to loss of flexion or extension. Excess fibrous (scar) tissue formation, or new bone (osteophyte) formation, around the graft can produce a mechanical block to extension. This complication is irrespective of graft choice.
GENERAL COMPLICATIONS
Infection
Despite surgery under sterile conditions, infection is still a potential complication of all operations. Post-operative infection maybe:
a) Superficial wounds only and usually settles with antibiotics.
b) Deep, involving the joint. Requires further surgery to washout the joint and intravenous antibiotics. May lead to joint stiffness and early degeneration.
Deep venous thrombosis & pulmonary embolus
A blood clot in the deep veins of the calf or thigh is a complication of any lower limb surgery. A blood clot that breaks-off and travels to the lungs is called a Pulmonary Embolus. This is a rare but life threatening complication. The treatment is anti-coagulation for 3-6 months.
Haemarthrosis
Bleeding within the knee joint can complicate any surgical procedure. A haemarthrosis will usually respond to ice, rest and physiotherapy but can lead to delayed recovery and joint stiffness.
Nerve injury
Small areas of numbness may be associated with the operative incisions. The numbness is usually temporary. Occasionally wounds can become painfully sensitive, although this normally settles with time.
Reflex sympathetic dystrophy
Reflex Sympathetic dystrophy is a little understood condition, which can complicate any operation. It consists of regional pain, swelling, sweating and stiffness due to local overactivity of the sympathetic nerves triggered by surgery, however minor.
Compartment syndrome
rare complication where fluid used to dilate and irrigate the knee joint tracks into the muscle compartments of the calf. Increased pressure within the calf can compromise the nerve and blood supply of the lower leg and requires emergency surgery to decompress the leg. This complication is irrespective of graft choice.
Potential complications of knee arthroscopy
Rhidian Morgan-Jones
Infection
Despite surgery under sterile conditions, infection is still a potential complication of all operations. Post-operative infection maybe:
a) Superficial wounds only and usually settles with antibiotics.
b) Deep involving the joint. Requires further surgery to washout the joint and intravenous antibiotics. May lead to joint stiffness and early degeneration.
Deep venous thrombosis & pulmonary embolus
A blood clot in the deep veins of the calf or thigh is a complication of any lower limb surgery. A blood clot that breaks-off and travels to the lungs is called a Pulmonary Embolus. This is a rare but life threatening complication. The treatment is anti-coagulation for 3-6 month
Haemarthrosis
Bleeding within the knee joint can complicate any surgical procedure. A haemarthrosis will usually respond to ice, rest and physiotherapy but can lead to delayed recovery and joint stiffness.
Wound healing
Although arthroscopy is performed through ‘Key Hole” incisions there is still a possibility of delayed wound healing. This may results in a serous discharge from the wounds for a short period after surgery and usually settles spontaneously. Occasionally the arthroscopy portals can produce a small local hernia of fatty tissue from within the knee. This rarely causes any clinical problems.
Nerve injury
Small areas of numbness may be associated with the operative incisions. The numbness is usually temporary. Occasionally wounds can become painfully sensitive, although this normally settles with time.
Reflex sympathetic dystrophy
Reflex Sympathetic dystrophy is a little understood condition, which can complicate any operation. It consists of regional pain, swelling, sweating and stiffness due to local overactivity of the sympathetic nerves triggered by surgery, however minor.
Compartment syndrome
A rare complication where fluid used to dilate and irrigate the knee joint tracks into the muscle compartments of the calf. Increased pressure within the calf can compromise the nerve and blood supply of the lower leg and requires emergency surgery to decompress the leg.
Infected total knee replacement
Infection is probably the worst complication of Total Knee Replacement. Infected Knee Replacements can lead to pain, loss of function and general ill health.
Eradicating the infection requires 1 or 2 further operations; the first to remove the infected joint and clean the bone surfaces and the second to reconstruct the joint with another permanent replacement. Between operations a temporary joint is inserted to allow patients to mobilise and go home in comfort. In selected cases and with high volume, experienced surgeons, infection can be cleared and the knee revised in a single operation.
Mr Morgan-Jones has pioneered revision of infected knee replacements in the UK and provides a regional and international service. Eradication of infection is achieved in 90% of patients under his care in a single operation. Many patients referred to Mr Morgan-Jones have had several revisions beforehand. The technique of re-revision requires sub-speciality skills that very few surgeons Worldwide can offer.
A full list of peer reviewed publications can be found on the CV.
Revision total knee replacement
Revision Knee Replacement: A future epidemic for which we already have solutions.
Primary total knee replacement in many studies offers greater than 90% survival of the implants at 15 years. Knee replacement is a highly successful operation with over 75,000 operations performed in the UK yearly (National Joint Registry). Every year over 5,000 knee replacements needed revision. The 2 commonest reasons for failure are infection, loosening and instability/stiffness. As the number of knee replacements increases, inevitably the number of revision operations will also increase.
Revision knee replacement involves opening the joint, removing all the components, cleaning out any plastic or metal debris and rebuilding the joint using metal stems and augments to support the new knee replacement. Revision knee replacement requires longer operative time, longer length of hospital stay, greater blood loss and diminished function have all been reported with revision compared with primary joint replacement. The survival rates following revision total knee replacement decrease with time, the importance of revision surgery being performed by high volume, specialist knee surgeons cannot be over emphasised.
CAUSES OF FAILURE
Infection
Infection in a prosthetic joint is a major cause of early failure and significant suffering for patients. Infection can be broadly divided into two categories. Firstly, and counting for the vast majority, is infection at the time of surgery. Secondly and much less common is late infection caused by organisms in the blood stream (bacteraemia) settling on a joint replacement.
Introduction of organisms at the time of surgery can never be totally excluded. There are, however, many precautions which can lower the risk significantly. These include an experienced specialist surgeon, operations performed within a ‘clean air enclosure’, dedicated theatre and ward staff, surgical time less than one hour, minimal disturbance of the post-operative dressings and lastly (and definitely least) antibiotic cover (prophylaxis).
Late infection resulting from blood borne infection, again, can never be totally excluded. However the risk is minimised by antibiotic cover at the time of other surgical interventions e.g. dental root canal work, abdominal or bladder surgery. Antibiotics are also indicated if there is a proven infection either in the same limb as the knee replacement or elsewhere.
Infected knee replacements present with pain, swelling, loss of movement, localised redness and warmth and occasionally a discharging sinus (a link between the joint and the skin that drains pus). Infection should always be excluded as a cause of failed joint replacement.
Loosening
With time all implants will loosen i.e. break the bond between the cement or implant and bone. This can occur late (10 to 15 years) merely as the result of time and activity. Unfortunately some joints loosen early (2 to 5 years) as a result of poorly positioned or poorly balanced implants at the time of surgery. Poorly positioned or balanced implants will result in excessive wear of the polyethylene liner and abnormal loading of the fixation to bone. The result will be loosening of the implant which may present with a variety of symptoms. These include: Pain from the loss of fixation to bone; Instability due to loss of polyethylene thickness and/or subsidence of the implants; Swelling caused by polyethylene and/or metal debris within the joint.
Stiffness
Stiffness results from two causes. Firstly, arthrofibrosis (excessive scar formation within the knee joint). This can be a natural phenomenon but is exacerbated by poor patient compliance with post-operative physiotherapy. The second cause of joint stiffness is a poorly balanced replacement i.e. the implants are poorly sized and positioned and result in inappropriate tension of the knee ligaments and capsule. Stiffness is often, but not always, accompanied by pain and significant loss of function.
Instability
Instability has 2 main causes. Ligament/soft tissue failure resulting in a knee with excess/abnormal and uncontrolled movement – the knee feels unstable. Secondly, a poorly balanced replacement i.e. the implants are poorly sized and positioned and result in inappropriate tension of the knee (the reverse of stiffness).
RESOLVING THE CAUSES OF FAILURE
Infection
An infected total knee replacement cannot be resolved by antibiotics alone. Rarely in an acute early infection, the joint can be salvaged by surgical debridement, lavage and exchange of the polyethylene liner.
More commonly an infected knee replacement will require two operations to eradicate the infection. In the first operation the knee replacement and all infected tissue are removed. A temporary joint replacement is constructed to allow the patient home, mobilising freely whilst the wounds and soft tissues settle. The second stage is then planned to permanently rebuild the joint. The timing of the second operation will depend on the type of temporary joint used and the confidence that the infection has been cleared. Historically infected knee replacements have been treated by inserting a spacer of acrylic cement. This meant that patients were often hospitalised and immobile for greater than 6 weeks. The timing of the second operation being determined by the incapacity of the patient, rather than certainty that the infection has cleared. Surgery performed at or around 6 to 8 weeks being performed before the soft tissues have recovered from the first operation, thus increasing the risk of recurrent infection.
Mr Morgan-Jones has pioneered single stage revision surgery in the UK. In selected cases, clearance of the infection and reconstruction with a new knee replacement can be performed in one operation.
Stiffness & instability
Stiffness of a knee resulting from arthrofibrosis may respond to physiotherapy, hard work and time. Failure to improve over 6 to 12 months should be considered for surgical excision of scar tissue with significant improvement expected.
Stiffness or instability resulting from malpositioning of the knee replacement will not improve with physiotherapy over any length of time. Malpositioning can only be improved by removing the replacement and revising the knee to establish soft tissue balance thus allowing the knee to move.
Loosening
A loose knee replacement can only be resolved by removal of the implants and revising the knee. Usually the revision will need stems to increase the surface area over which fixation to bone can be achieved. Augments will be required to restore the joint line and stabilise the soft tissues and ligaments. The cause of joint loosening should be established before surgery. Infection in particular should be excluded.
Example
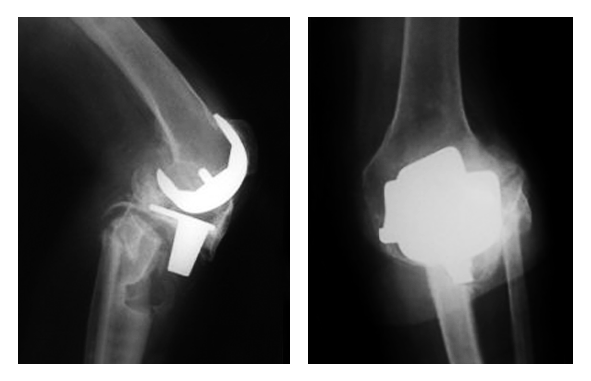
An 81 year old man presented five years after breaking his leg beneath a total knee replacement. The broken leg resulted from loosening of the knee replacement produced by polyethylene and metal debris from the failing joint. The surgeons treating the initial break were unable to offer a revision operation and advised a brace and crutches. The X-rays below show the loose knee replacement, bone cyst beneath the joint and the unhealed break.
After five years on crutches the patient was referred by his General Practitioner to the specialist knee replacement clinic in Cardiff. The knee was successfully revised using a hinged joint with long uncemented stems to bypass the bone defect and the unhealed fracture. The patient walked out of hospital five days after the operation and was off crutches by six weeks.

Conclusion
Total knee replacement is an excellent operation for pain relief and return of function. However, as increasing numbers of knee replacements are performed each year the number of failing joint replacements will also increase. Revision knee replacement is a specialised operation with good long term results when performed by experienced knee surgeons in dedicated units.
T. 029 2043 6300 E.[email protected]
T. 029 2043 6300 E.[email protected]